Metabolic confusion affects energy, fat, protein, and hormone metabolism by periodically changing calorie intake. In the short term, body weight can decrease by 4%-6%, but in the long term, it may lead to inflammation, decreased insulin sensitivity, and waste metabolism disorders, with a reduction in basal metabolic rate by 8%.
Energy and Glucose Metabolism Disorders
Metabolic confusion, or the method of influencing metabolism by periodically changing calorie intake, has received increasing attention. The core concept underlying this is preventing the body from adapting to a fixed low-calorie state, thereby maintaining a higher metabolic rate through frequent changes in calorie intake. Energy metabolism disorder is one of the major concerns with metabolic confusion. Energy metabolism in the human body refers to food transformation into usable energy, maintains basic life activities, and consumes energy daily.
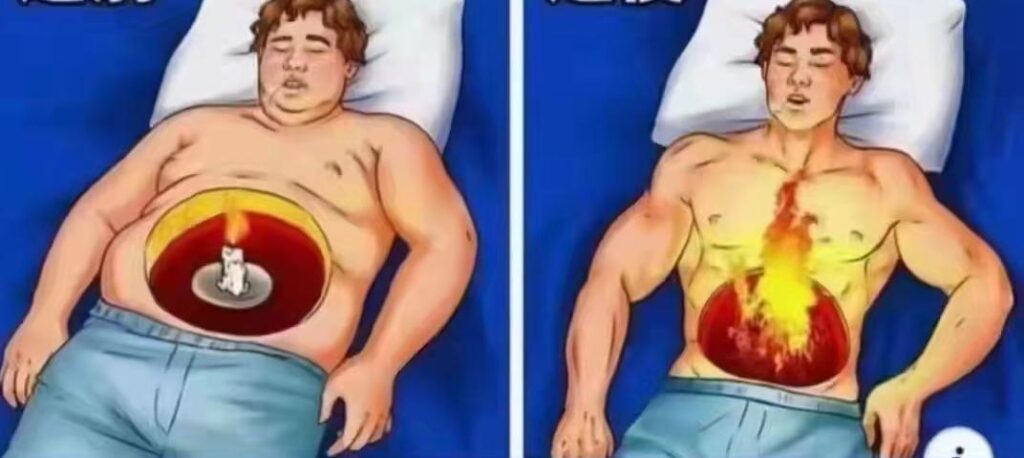
The fundamental idea of metabolic confusion is that a very low-calorie diet for an extended period reduces the basal metabolic rate, thus putting the body in an “energy-saving mode.” During this time, less energy is consumed, and the speed of weight loss slows down. By periodically changing calorie intake, the body cannot adapt to low-calorie intake, so energy expenditure remains higher.

Frequent fluctuations in calories do not entirely stop the decrease in basal metabolic rate. One study found that within the first four weeks, individuals on a metabolic confusion diet experienced an average weight loss of approximately 4%. Later, basal metabolic rates decreased by about 8%, gradually weakening the effect of weight loss. Another study reported that, within a 12-week metabolic confusion diet, subjects lost 5%-6% body weight in the first six weeks, but in the following six weeks, the rate of weight loss significantly reduced, showing that the body gradually adapted to fluctuating calories. While metabolic confusion might enhance energy expenditure in the short term, it is limited by the body’s metabolic adaptation in the long term.
Another major factor of metabolic confusion is glucose metabolism disorders. Glucose metabolism refers to the use and deposition of glucose in the body, which is a primary energy source, especially during high-intensity activities. The metabolic confusion diet involves fluctuations in carbohydrate intake, significantly affecting glucose metabolism. When carbohydrate intake is reduced, the body minimizes glucose utilization and relies more on fat as an energy source. Frequent carbohydrate fluctuations can destabilize blood sugar levels and decrease insulin sensitivity.
A study showed that during a 12-week metabolic confusion diet, blood sugar fluctuations increased by 15%, and insulin sensitivity decreased by about 10%. This shows that although energy consumption may temporarily increase, the long-term effects on insulin regulation and glucose metabolism are negative. In some cases, fluctuations may cause more severe glucose metabolism problems. In a metabolic confusion experiment, during low-carbohydrate intake, insulin secretion dropped by 30%, while a sudden increase in intake caused insulin secretion to rise by about 25%.
These fluctuations can destabilize blood sugar, increasing the long-term risk of metabolic diseases, especially type 2 diabetes. Liver glycogen storage is also impacted by metabolic confusion. Glycogen, stored primarily in the liver, is mobilized when energy demand is high. Frequent calorie and carbohydrate changes disrupt the liver’s balance of glycogen storage and usage. When calories are low, glycogen is depleted; when calories increase, the liver may prioritize fat synthesis over glycogen replenishment, reducing metabolic efficiency.
Disorders in Fat and Protein Metabolism
Fat serves as the primary energy storage in the body, especially when calorie intake is insufficient. The body breaks down fat to produce energy. In a metabolic confusion diet, because of frequent changes in calorie intake, the process of fat storage and breakdown can become disordered. A study showed that fat breakdown increased by 20% on low-calorie days, while on high-calorie days, fat storage rose by about 15%. These fluctuations can lead to imbalances in fat metabolism and increase the risk of fat accumulation.
On low-calorie days, fat is broken down, while on high-calorie days, the body stores fat to prepare for future energy needs. Metabolic confusion may cause fat redistribution, particularly visceral fat accumulation. Visceral fat not only affects appearance but also raises the risks of cardiovascular disease and diabetes. In a 12-week study, visceral fat content increased by an average of 10%, suggesting potential long-term health risks.
Protein is essential for maintaining and repairing body tissues, including muscles, skin, and hair. In a metabolic confusion diet, protein utilization may decrease, leading to imbalances between muscle protein breakdown and synthesis. A study found that muscle protein synthesis decreased by about 15% in the low-calorie phase, and although protein synthesis recovered in the high-calorie phase, it was still 10% lower than in constant-diet groups. Muscle loss reduces basal metabolic rate, making it harder to lose and maintain weight. Metabolic confusion may also disrupt nitrogen balance, a key measure of protein metabolism. In the low-calorie phase, nitrogen excretion increases, indicating protein breakdown for energy. Long-term negative nitrogen balance can lead to muscle loss and metabolic dysfunction.
Hormonal Imbalance
Hormones regulate physiological processes and play a key role in energy balance and metabolism. While metabolic confusion aims to “reset” metabolism by changing calorie intake, it can cause hormonal disruptions. Insulin, which helps regulate blood sugar, may become unstable due to frequent changes in calorie and carbohydrate intake. A 12-week study found that insulin sensitivity decreased by about 12%, particularly after consuming a large amount of carbohydrates. This leads to greater blood sugar fluctuations and an increased risk of type 2 diabetes.
Leptin, which regulates appetite and energy balance, is also impacted by metabolic confusion. During low-calorie phases, leptin levels dropped by 30%, and although leptin partially recovered during high-calorie phases, energy expenditure remained low. Cortisol, the “stress hormone,” also increases during low-calorie days, signaling the body to conserve energy. In an 8-week study, cortisol levels increased by about 15% during low-calorie phases. Thyroid hormones, especially T3, which regulates basal metabolic rate, decreased by 22% during low-calorie intake, reducing energy expenditure. Although T3 levels recovered in the high-calorie phase, basal metabolic rates did not return to initial levels. Growth hormone, which preserves muscle and mobilizes fat, increased by 18% in the low-calorie phase but dropped by 12% in the high-calorie phase.

Inflammation and Waste Metabolism Disorders
Chronic inflammation can lead to metabolic disturbances, and metabolic confusion can induce low-grade chronic inflammation due to frequent calorie fluctuations. In one study, participants’ C-reactive protein (CRP), a marker for inflammation, increased by about 20% during low-calorie phases. Chronic inflammation can damage insulin receptors, decreasing insulin sensitivity and increasing the risk of type 2 diabetes. After several calorie fluctuations, insulin sensitivity decreased by about 15%, and inflammation markers remained elevated.
Metabolic waste products, such as free radicals, accumulate in the body and are processed by the liver and kidneys. Frequent changes in calorie and nutrient intake can reduce the body’s ability to handle these wastes, leading to the accumulation of harmful substances. Free radicals can attack cell membranes, proteins, and DNA, causing oxidative stress and damage. A study showed that antioxidant enzymes decreased by about 18%, while free radical production increased by 25% during low-calorie phases.
Metabolic confusion can also increase the liver’s workload during low-calorie days, when it must break down stored fat for energy. Liver function markers (ALT) increased by about 10% during low-calorie phases, indicating an increased metabolic burden. Lactic acid, produced during anaerobic metabolism, accumulated by 30% during low-calorie phases, leading to muscle fatigue and impaired performance. High-protein intake days increased blood urea nitrogen by about 15%, which increased the kidneys’ metabolic burden.